Jeff Henderson remembers the day he finally went to get tested for acquired immune deficiency syndrome. He was living in Washington, D.C., in the mid-1980s and was experiencing classic symptoms of AIDS: swollen lymph nodes, fatigue, and acute body aches. As it happened, Henderson, then a young man working for a federally funded housing program, lived near a well-known provider of AIDS services called the Whitman-Walker Clinic. But Henderson had a hard time getting himself through the door. He walked around and around the block, nervous—not only about the results.
Henderson is African American. So, largely, was the neighborhood around the clinic, the neighborhood where he lived. Yet the clinic’s clientele was mostly white, gay men. Henderson worried: If his neighbors saw him walking in, what would they think?
He eventually did get tested and found out he was infected with the human immunodeficiency virus (HIV) that causes AIDS. But it has taken him a long time to get where he is today, sitting in his Seattle living room—cluttered comfortably with potted plants, African fabrics, and books by African Americans such as bell hooks—talking openly about his disease.
Henderson’s longtime reluctance to talk about his illness is shared by many in the African-American community, where AIDS often is thought of both as a white, gay disease and as God’s punishment. Consequently, many have failed to notice a remarkable demographic shift in the AIDS epidemic: If it once made sense in this country to talk about AIDS as a white, gay disease, it does no longer. Today, if anything, AIDS is turning into a black disease.
Since 1996, African Americans have accounted for a greater share of new AIDS cases nationwide than any other racial group. In 2000, the latest year for which data are available from the federal Centers for Disease Control (CDC), African Americans represented 49 percent of reported cases, although they make up only 12 percent of the population. Whites accounted for just 30 percent of cases.
African Americans account for an even greater proportion—a majority—of new HIV diagnoses: an estimated 54 percent, according to the CDC.
Neither black nor white communities generally recognize the new demographics, says Phill Wilson, executive director of the African American AIDS Policy and Training Institute in Los Angeles. “Every time I tell people that, they’re absolutely shocked,” he says.
Locally, the number of African Americans with AIDS is not as high, given that less than 4 percent of the state’s population is black. Even so, African Americans account for 17 percent of both AIDS and HIV cases reported in the state between 1998 and the present, a figure representing more than four times their share of the population.
The numbers come as no surprise to public-health professionals. Dr. Helene Gayle is a former head of the CDC’s AIDS program who now directs AIDS-related giving at the Bill and Melinda Gates Foundation: “The first time we wrote about it in a report was 1985. Even at that time, there was a disproportionate impact—25 percent of AIDS cases were among African Americans.”
The epidemic was simply going where epidemics usually go, she explains: into “communities of the disenfranchised”—those with poor access to health care, high rates of drug use, and other social burdens that fuel disease.
Yet at the highest political levels, there sometimes have been reasons for turning a blind eye to this phenomenon. Al Jonsen, a retired chair of the University of Washington’s department of medical history and ethics, headed a National Academy of Sciences committee that in 1993 produced a report predicting the rise of AIDS in communities of color. In an e-mail, Jonsen remembers that the report “was severely criticized by Dr. David Rogers,” then vice chair of the National Commission on AIDS, “who feared that our message would jeopardize the current political approach to getting AIDS funding, namely that the epidemic was a threat to all citizens equally.”
At a Seattle conference recently, Jonsen elaborates that Rogers felt “he was only able to get funding from Congress if congressmen from Iowa or wherever felt that the kids from his district were going to get AIDS.” In other words, AIDS couldn’t be seen as too black, just as it couldn’t be depicted as exclusively gay. Jonsen says that the report was denied any impact on social policy, and “of course, what we predicted ended up happening.”
Even with the numbers as bad as they are now in the African-American community, though, those concerned with the issue are still fighting for attention. “It’s just not a major issue in our community,” says Kiande Jikada, an outreach worker at the People of Color Against AIDS Network (POCAAN), which is the major organization in town catering to African Americans with the disease.
Quinten Welch, executive director of another AIDS organization, the Seattle Treatment Education Project, agrees, even as he plans an African-American summit next month, the second put on by his organization. “You know, there are a lot of issues in the African-American community,” he explains. It’s hard to add one to the already crowded agenda—particularly one that might make some people say, in the words of Welch, “This is yet another thing that is linked to your community.”
Yet linked to the community it is, and African Americans had better come to terms with it, warns Doug Austin, a local black AIDS activist who has the disease himself. “We’re in a state of emergency.” THE LINK BETWEEN epidemics and demographics is a tricky matter, and not just politically. Bringing something like AIDS into the spotlight can prompt those at risk to take precautions, but it can also dissuade others from doing so. One reason AIDS has gotten as far as it has in the African-American community, health workers say, is because of the previous labeling of AIDS as a white, gay disease. Many African Americans have thought they didn’t need to pay attention to prevention, even when their risks of infection were high.
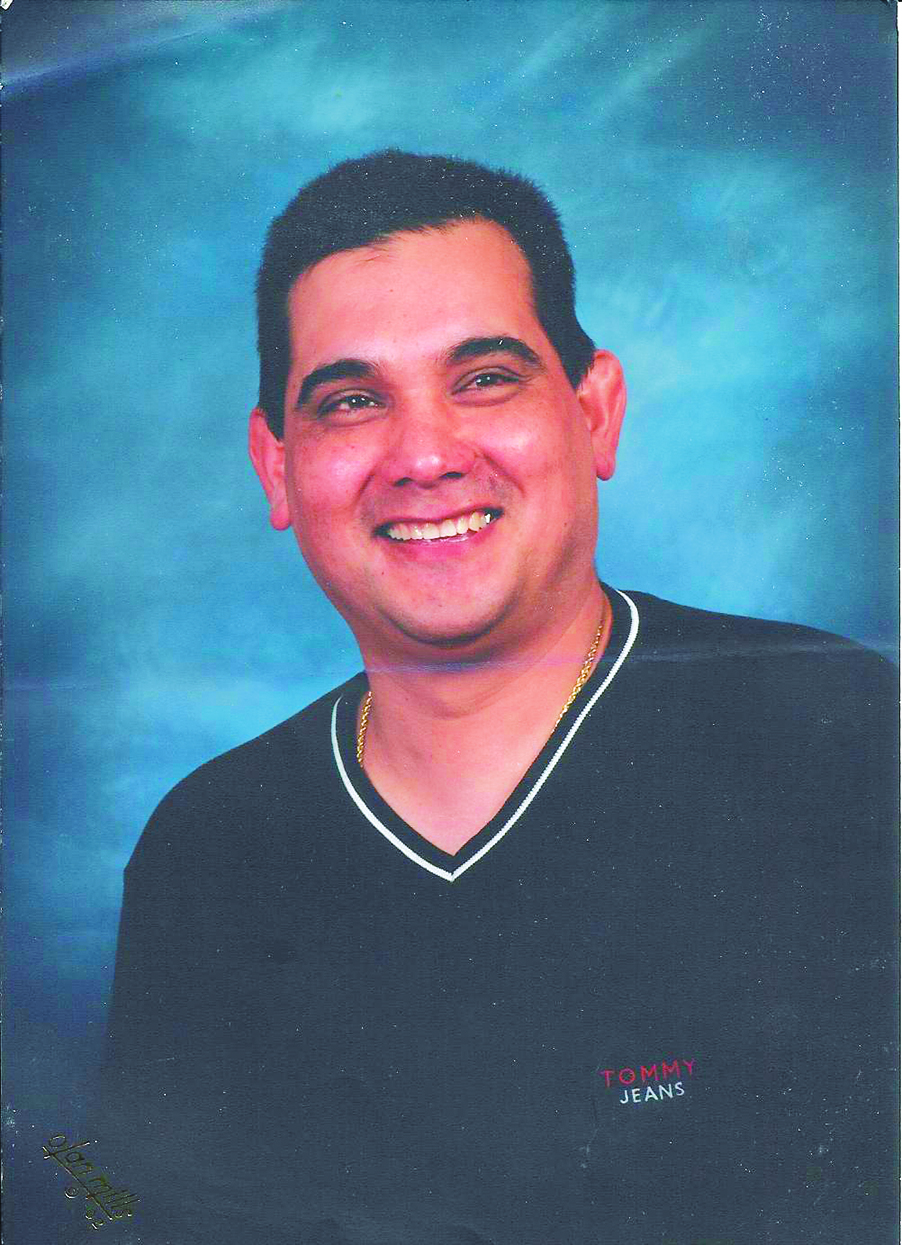
If anyone should have been practicing safe sex, for example, it should have been Jeff Henderson. Now 44, Henderson is a well-kempt, well-spoken man who radiates the kind of eagerness for human warmth often shared by those who have been on the verge of death. Five years ago, he underwent chemotherapy for AIDS-related cancer and was in a wheelchair. Anti-retroviral drugs have now filled out his body and given him enough vigor to get around the city by bicycle.
But in the mid-1980s, back in Washington, D.C., Henderson was a high-living young man. Bisexual and on a quest to “bring together the perfect man and the perfect woman” in a three-way relationship, Henderson was living with a woman and openly having affairs with men. On top of that, Henderson was taking speed intravenously as part of a hardworking, hard-partying crowd of D.C. do-gooders.
It was a double whammy of risk: having sex with men and I.V. drug use. But Henderson continued to have unprotected sex, never considering that he might infect his girlfriend as well as himself. “Our understanding back then was that it was kind of a gay thing,” he says of AIDS. And even if he were to become infected by having sex with men, he didn’t think he could pass the virus through heterosexual contact. “We didn’t think it was a problem,” he says.
It wasn’t until his girlfriend got pregnant that they realized that not only they, but their unborn child, were at risk. Their baby was not infected, but both Henderson and his girlfriend were.
It might have been looking at AIDS as a “gay thing,” rather than a white thing, that helped trip up Henderson. But among many African Americans, gay is perceived to have a color, and it’s white. Henderson recalls getting a hate call during Gay Pride Week a few months ago, when he advertised an event for black gays in The Facts, one of Seattle’s African-American newspapers. “You need to take that gay shit and keep it in the white community where it belongs,” the caller hissed. Hinted at in the caller’s venom was a notion that being black and gay is a kind of assimilation, even selling out.
In large part, too, the stigma of homosexuality derives from the traditional religiousness of the African-American community. One time a few years ago, Henderson was visiting his mother’s church in Tacoma when the pastor called him into his office and gave him what he calls the “Adam and Steve” speech: “God didn’t create Adam and Steve, he created Adam and Eve.”
POCAAN’s Jikada says homosexuality is also seen as “a last break in masculinity” for black men, after centuries of being torn down. So, Jikada and others say, many African Americans who have sex with other men don’t identify as gay or bisexual (the classic case being men in jail), either to themselves or to the world. Many have wives or girlfriends. Such men are said to be “on the down low,” and it is an existence that has implications for the spread of AIDS. The term is used as the name of a newsletter targeting African Americans put out by the Lifelong AIDS Alliance. Men who see AIDS as a gay disease and don’t consider themselves gay have tended not to take precautions.
Even those who know they’re at risk, if they’re in the closet, might not use condoms with their wives or girlfriends because of the questions it would raise. That’s how homosexual transmission often leads to heterosexual transmission among African Americans. AIDS activist Austin says that’s how unsuspecting black women end up with the disease, “because somebody lied to them,” and so they might have an advanced form of the disease when they find out. “The woman has no ordinary reason to feel like she should be tested, so she doesn’t until her health is really in jeopardy.”
IT WOULD BE A MISTAKE, however, to assume that gay sex (with its tangential effect on the straight population) is the driving force behind AIDS among African Americans, as it is among whites. About a quarter of blacks with AIDS nationally were infected through homosexual contact. The biggest means of transmission, accounting for 36 percent of cases among blacks, is intravenous drug use. Austin himself is an example. “I always say I had four careers,” the bald 51-year-old recounts one day in his South Seattle apartment. Looking drained by his illness but roused by the subject to sharp observations, Austin says, “First, I spent 10 years as a firefighter and paramedic in Bellevue,” a pioneer—only the second black person to graduate from the University of Washington’s paramedic training in 1978. “For the next 10 years, I was the program coordinator for all the emergency medical services at the county.” It was an excellent job with a lot of responsibilities. But it was also stressful.
Meanwhile, his personal life was turning more stressful as well. His brother and sister were having problems, so he took in their four children, though he already had four of his own. Then his wife had a stroke. She survived, but had to re-learn everything. When his mother died a few years later, he went over the edge and into his third career—as a drug addict.
“It didn’t start out sharing needles,” he says. “But when you get to the point where you have an addiction, you don’t care whether the needles are dirty or not. You just want the drugs.” Of course, he should have known better. “I was a medic, my god,” he says plaintively, the bitter irony seeming to strike him anew. “I had helped put together the HIV training program for the state.” That program trained paramedics in precautions for handling patients with AIDS.
Two years into shooting up, he found out he had AIDS and lost everything, including his family. He did, however, find a fourth career—as an AIDS activist. He joined King County’s HIV/AIDS Planning Council and became a peer supporter at POCAAN.
“I don’t know how much time I have left,” Austin says. His body is wracked by an AIDS-related case of hepatitis C. “I want to do as much as I possibly can to see the rates of infection start dropping.”
Austin was lucky in one way: He didn’t pass the virus on to his former wife of 22 years. Other drug users do, further fueling heterosexual transmission among African Americans.
That might be how Madeline Brooks-Wyatt ended up with AIDS. An extroverted 44-year-old with a cascade of red extensions piled atop her head and a warm, deep voice, Brooks-Wyatt had taken her ex-husband back after a period of separation when she found out she was infected.
Brooks-Wyatt heard that during their separation, while she was living out of state, her now-deceased ex had “gone wild for his drugs,” wild with the women, too, for that matter. Deciding to give him another chance anyway, she soon observed him undergo a mysterious transformation. “He was cold all the time and had night sweats. And he was in a lot of pain; he was like, ‘Don’t touch me, leave me alone.’ He would just close himself up in his room”— sometimes for weeks at a time. “And he had this body odor that turned my stomach.”
She pleaded with him to go to the doctor. He refused. Eventually, she went to the doctor, because she was noticing some strange symptoms in herself, including the swelling of lymph nodes on the side of her neck. “To me, I looked like Frankenstein’s wife.” The doctor gave her every test in the book before she reluctantly asked Brooks-Wyatt to take an HIV test.
When Brooks-Wyatt told her man the results, she says, he accused her of infecting him. It’s not an uncommon pattern, AIDS workers say, but it infuriated Brooks-Wyatt. She says she was spending all her time at church, where she served as choir director. “I didn’t have no time to mess around.”
AS SICK AS HE WAS, why didn’t her former husband go to the doctor himself? It could be he didn’t want to hear the bad news. But another factor could also have come into play: the wariness with which many African Americans greet the medical profession. There’s the financial element, certainly. Because proportionately fewer African Americans are insured, doctor visits can be prohibitively expensive, as would be prescription drugs.
Steve Wakefield, a longtime advocate for African Americans with AIDS, has written about another barrier that sometimes keeps blacks from getting tested and from continuing with treatment once they are. Traditionally, most AIDS services have been oriented toward white, gay men. “And that’s probably the hardest part of beginning to deal with HIV as a person of color: being forced to move in a new world on account of your HIV status,” Wakefield writes in a publication called There Is Hope: Learning to Live With HIV.
That’s not all, however. Perhaps most damaging for the medical profession’s reputation in the African-American community are the infamous Tuskegee experiments, in which, for research purposes, scientists watched poor blacks die from syphilis, even though an effective penicillin treatment had been developed.
That’s a legacy Wakefield confronts constantly in his current job as head of community education for the HIV Vaccine Trials Network, the worldwide collaboration of research centers coordinated by the Fred Hutchinson Cancer Research Center in Seattle.
His office is on a sprawling floor at the Hutch. On the wall is a big map stuck with pins showing the locations of the centers, including Pune in India, Sao Paulo in Brazil, and Soweto in South Africa. Wakefield, a burly African American, shakes his shaved head and laughs when asked if Tuskegee comes up as he talks to African-American communities about the risks and benefits of the trials. “Every time, every city. I’ve never spoken to a black audience where it didn’t come up.”
In turn, he says, “When I go to potential research sites in Uganda or Botswana or Malawi, the minute I step down from the podium, someone comes up to ask a question: ‘How many black Americans are involved in the trials?’ They don’t want to do experiments in their country if we’re not willing to do it on black Americans.”
Researchers, in fact, are very willing to do it on black Americans. You might even say they’re desperate to, for one simple reason—as Wakefield explains, the trials need to reflect the epidemic. Because so many African Americans are infected, scientists need to make sure that any vaccine developed will work just as effectively on them as on anybody else. For instance, Wakefield says, “African Americans have a propensity for sickle-cell anemia.” Could that possibly be a factor in how a vaccine will affect their immune system?
You need to appreciate, however, just how tough Wakefield’s job is. Not only is there the Tuskegee legacy, but these particular clinical trials are different than most. Most trials ask people who are already sick to come in. But these, as vaccine trials, are about prevention. Scientists ask participants who are perfectly fine to have something shot into them repeatedly.
No, subjects aren’t then infected with HIV to see if the vaccine works, to answer a question frequently asked of Wakefield. In early trials, scientists just want to gauge the safety of the vaccines and their effect on the immune system. Later, researchers will look for high-risk subjects, like I.V. drug users, who are likely to be exposed to the virus themselves. Still, that’s quite a hard sell for anyone, not just blacks. Even harder because the substances tested, in the way that vaccines work, trick the immune system into thinking the body has the virus, thus creating antibodies. Unfortunately, it also tricks the conventional AIDS test, which measures such antibodies as a means of finding out if you have the virus—generating a result that could be frightening.
The participation rate among African Americans isn’t bad, considering. Twelve percent of the subjects in the network’s largest trial are African Americans, proportional to their representation in the population. Still, when you consider that the majority of new infections are among African Americans, Wakefield says, “we haven’t done the job we need to do yet.”
Locally, where just 3 percent of vaccine participants since 1988 have been African Americans, researchers are starting to recruit blacks more aggressively. In May, the University of Washington’s research center for the first time placed an ad in The Facts seeking participants. For maximum impact, though, says Dennis Torres, the local center’s community educator, “it’s really about getting into the churches.”
AGAIN AND AGAIN, AIDS professionals and activists stress the importance of mobilizing churches, the traditional center of black life, in the fight against AIDS. But persuading black churches hasn’t proved easy, in large part because AIDS has long been linked with the taboo of homosexuality. In January, Brooks-Wyatt took a job at POCAAN as a church liaison. Seeking to involve churches in educational work, she sent a letter explaining her mission, inviting pastors to contact her. She heard nothing. Then she phoned pastors and left messages. Not one called her back.
Frustrated, she has a new plan: “I won’t be calling anymore. I’ll be showing up.”
The Multifaith AIDS Project, known as MAPS, has had a similar experience trying to recruit care teams in black churches. Each team acts as a support system for one person with AIDS, doing such things as driving that person to doctor’s visits, running errands, and celebrating birthdays. Of the organization’s 40 care teams, only two are in African-American churches. “I don’t know the best way to get past it, I just don’t know,” says MAPS program director Trudy James.
Still, there are those teams at two black churches, First African Methodist Episcopal Church and Mount Zion Baptist Church, although they haven’t been supported as well as one might hope. Charlotte Ruff, a founding member of First AME’s team, says members of the congregation seem glad it’s there but aren’t necessarily volunteering to help. “I wouldn’t say it’s in the forefront of activities,” Ruff says, adding that she’d like to see the church have more teams. “There’s such a big need in the African-American community, and each team can only take care of one person or family.”
Similarly, Kenny Joe McMullen bemoans the fact that the care team he heads at Mount Zion has only four members. Parishioners look to their pastor for priorities, McMullen says. “If the pastor does not legitimize or make something an urgent matter, if it’s not something he’s pushing, parishioners will not rally behind it.” And that’s what McMullen says has happened at Mount Zion, whose high-profile pastor, the Rev. Dr. Leslie D. Braxton, has put his energies into more conventional civil-rights issues, helping, for instance, to shut down part of Interstate 5 last spring after the fatal police shooting of a black man.
McMullen notes that Braxton has shown more interest in the matter after a trip this summer to South Africa, where, like all of sub-Saharan Africa, the impact of AIDS on blacks is impossible to ignore. At the pulpit on a recent Sunday, he spoke about the need to establish AIDS ministries. (Braxton didn’t return phone calls seeking comment.) And, in fact, Carolyn Dukes, the head of Mount Zion’s health ministries, is trying to put together a new support group for people with AIDS, which she hopes will be headed by a deacon.
There are other signs that AIDS awareness is growing in the black community. “When you think of HIV and AIDS, I’m not sure people will think, ‘That’s the Urban League,'” says the organization’s Seattle president, James Kelly. Like Braxton, the Urban League has been preoccupied with classic civil-rights concerns. With the civil-rights battle not what it once was, however, and the Urban League looking for relevancy in the 21st century, Kelly says he is watching for ways to get involved in the AIDS fight. “We have to put energy into creating an [AIDS] agenda, just like we put energy into getting the right to vote,” he says.
For the Urban League, Kelly says, the trick is finding a unique contribution to make amidst all the other groups working on AIDS, while not eclipsing the organization’s “bread and butter” issues. One approach might be concentrating on the lack of access to health care faced by many African Americans.
AIDS groups are stepping up their services to African Americans, too. There’s the African-American summit planned for next month by the Seattle Treatment Education Project. There’s also a new program run by an offshoot of POCAAN, called Brother to Brother, that takes advantage of barbershops as a mainstay of African-American life by training black barbers to educate their patrons about AIDS.
Meanwhile, POCAAN has been running, for the past three years, a support group and referral service for African Americans with AIDS called KONNECT II. The group meets on Wednesday nights over dinner. On a recent night, a restaurant has donated Cornish hens, wild rice, fruit salad, and thickly frosted chocolate cake. About a dozen people take their plates and settle in around a conference table at POCAAN’s Rainier Valley office, ready to listen to a psychologist speak about how her profession can help people with AIDS.
To look around the table is to be reminded that this is the new face of AIDS, not one we’re used to seeing. Attending are a former drug user, a bisexual man, and a woman who believes she became infected through her husband, along with Austin, Henderson, and Brooks-Wyatt. Here also are two women with their children.
One of the mothers is making funny faces at her small baby, who is wrapped in a blanket lying in front of her on the table. As the participants go around the table introducing themselves, she informs the group that her little girl is, thankfully, HIV-negative.
As for herself, she says that she just got the results of a blood test that measures the strength of the body’s immune system by the number of white CD4 cells. “I’m sorry to say,” she says, pausing dramatically before throwing her hands up in the air jubilantly, “my CD4 count is 900.” It’s a high number, well within the normal range for an adult.
She declares: “I feel like Stella trying to get my groove back.”