AS THEY CONTINUE to negotiate a long-predicted $20 million to $30 million civil fine for Medicare billing fraud, University of Washington and federal officials are keeping the record sealed on how, exactly, UW doctors submitted millions of dollars worth of faulty medical insurance reimbursement claims from 1996 to 2002. But former UW neurosurgeon H. Richard Winn, convicted of a felony related to the billing scandal, is revealing some of the answers in a medical journal article he wrote recently. He says the four-year federal probe, sparked by a 1999 whistleblowers claim, involved five areas of non-compliance by the university and that violations included charging for hundreds of operations that were retroactively billed to Medicare. The UW also charged taxpayers for bedside procedures by doctors who werent at bedsides and for surgical procedures doneat least according to the paperworkin the absence of surgeons.
The feds tried but failed to make a case for criminal charges, as well, against the School of Medicine, Winn says, then belatedly discovered that Medicare apparently approved the practices the FBI was investigating. Ultimately, criminal charges were brought against just Winn and a second doctor, but no top school officials.
As part of his sentence, Winn was ordered to write a cautionary article on the pitfalls of billing for Medicare, Medicaid, and military Tricare insurance reimbursements. It appears in the January issue of the Journal of Neurosurgery, but his revelations have not been reported in mainstream media. In Winns view, most if not all of the questioned billings were the result of confusion and sloppy paperwork, not a willful heist of public money. The UW and its affiliated faculty medical/billing group, UW Physicians (UWP), have compliance staffs to deal with the voluminous Medicare billing bible, and they should have caught some of the errors, Winn says. But the real problem was a chain of errors and misunderstandings that began with top doctors who lacked billing know-howdespite a Medicare agreement each one signs that holds them individually responsible for errors or cheatingand medical staffers who often submitted incorrect data. The university, Winn says, was focused on the academic side of medicine and provided little oversight, resulting in an administrative wall between the medical school and the facultys billing agency.
HIS FEELING that inflated billings were mostly unintended mistakes is apparently widespread at the UW and likely one reason university officials, as first reported in the Seattle Post-Intelligencer on Monday, Jan. 19, are balking at settling the case for as much as $35 millionarguing that $20 million would be more fair. Prosecutors have said, however, that they believe many inflated billings rose above the level of misunderstanding, and some bills were for phantom services.
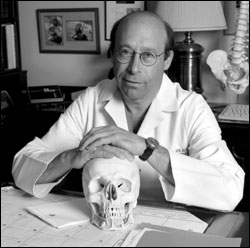
Winn, 60, who was also chief of Harborview Medical Center neurosurgery, last year was ordered to pay $500,000 and perform 1,000 hours of community service for obstructing the federal investigation. He took full responsibility, admitting he asked others to lie or conceal incriminating details and created an air of fear and intimidation (see Brain Damage, Jan. 15, 2003). Prosecutors conceded that the wrongful claims submitted by Winns department were not intended by the defendant to be fraudulent and were instead the product of mistake and confusion as to the meaning and application of the rules Described as a gifted neurosurgeon, Winn was forced to resign from the UW but got a separation deal that can bring him up to $3.7 million over five yearsan amount to be offset by any earnings Winn receives elsewhere. He is currently a researcher at Mount Sinai School of Medicine in New York, earning just under $50,000, according to The Seattle Times.
Winn has said little publicly about his conviction. But in the nine-page, court-ordered Journal of Neurosurgery article, he gets some mild revenge by suggesting, as his many supporters have insisted since he was first charged in 2002, that he took a fall for others. He also gently needles the feds for going after him. To put this $500,000 repayment] in perspective, he says, between 1996 and 2002 (the government subpoenaed records from this time period), the Department of Neurological Surgery billed approximately $90 million and received revenues of approximately $40 million. Thus the $500,000 repayment represented 0.5 percent and 1.3 percent of the billings and revenues, respectively. This percentage is below the threshold for investigation according to most auditing standards. Federal officials admit they made an example of both Winn and UW kidney specialist Dr. William Couser, who also pleaded guilty to criminal fraud last year and was ordered to pay back $100,000 for overbilling. They are the first university faculty members in the U.S. to be convicted of criminal Medicare fraud.
Winn says 55 percent of UW Physicians doctors were critical of their faculty billing groups operations, according to a 2002 questionnaire, especially in regard to financial information and training. He advises Medicare billers to follow the rule of international armament treaties: trust but verify. Its an important concept to guide the management of faculty practice plans and emphasizes the need for transparency in the activities of these organizations, he says. Faculty members must acquire a comprehensive understanding of health care regulations or face personal peril.
IN PURSUING possible criminal and civil violations, Winn says in the medical journal article, the feds struck out in two areas of their investigation. In one, the U.S. dropped its probe into suspected illegal billing for radiosurgery frame placement, Winn says. (Stereotactic radiosurgery involves high doses of radiation directed to a small area of the braina treatment so precise that a special frame is used to hold the head perfectly still.) The government contended that frame placement [by a junior attendant doctor rather than the attending physician] was the more important component, and because the attending did not place the frame in most cases, a fee was inappropriately submitted for radiosurgery cases. The feds simply didnt understand the procedure, Winn indicates, and, After an educational discussion, the government dropped this aspect of its investigation.
More seriously, the FBI and U.S. attorney were also attempting to prove the UW School of Medicine and UW Physicians committed criminal fraud by billing for services of Medicare-ineligible doctors still in residency, he says. But the UW ultimately produced a letter from Medicare that at least mitigated the suspected criminal intent. Winn, with apparent relish, says in the Journal of Neurosurgery article that though the long federal probe involved subpoenaing thousands of pages of documents and files from the department, the UW School of Medicine, the UWP, and the ABNS [American Board of Neurological Surgery], neither the U.S. Attorneys Office nor the FBI was aware of the [mitigating] contractual agreement Furthermore, they had not seen [a mitigating] letter from the associate dean for clinical affairs until the documents were disclosed to them in February 2002 by my attorney, Cyrus R. Vance Jr. His contention of a lack of criminal intent was not subsequently challenged.
WINN ADMITS, however, that those billings were submitted in error, presented in the name of neurosurgery residents who had wrongly been given faculty eligibility. Both the associate dean for clinical affairs and I erred in our assessment of eligibility, Winn says. Still, At no time was any question or concern raised by any of the department faculty either to my predecessors or to me in regard to the appropriateness of these faculty appointments. In the instance of a mass retroactive billingthe UW had discovered it could legitimately recover costs for earlier procedures it hadnt billed forthe school badly overreached, Winn says. Fees could be charged for complex surgical procedures but not minor ones. Unfortunately, he writes, individuals from UWP responsible for assembling the appropriate materials instead collected the charts of all patientsnot just those of complex caseswho had undergone treatment during the time period, and the [chief residents] then added the required language to all charts, even for minor procedures.
Ignorance of the rules and law contributed to errors in billing for bedside procedures, too, such as lumbar punctures or insertion of intracranial pressure monitors, Winn says. Previously, Medicare did not require a faculty doctor to be at bedside but only in the vicinity when a resident did the procedure. After 1996, an attending physician had to be, in Winns words, almost shoulder-to-shoulder to the doctor doing the procedure. Confusion, he says, about these new regulations persisted, and consequently fees continued to be generated in some cases in the absence of a shoulder-to-shoulder, elbow-to-elbow attending presence. (Federal officials have said that in one case a doctor was on vacation when his name was listed as the attending bedside physician; UW Physicians says it discontinued such billings in 2000.)
CONFUSION AND errant billing practices reigned in surgical cases, too, Winn indicates. The government contended that there were many surgical fees submitted for operative procedures performed in the absence of an attending surgeon based on the nursing operating room record. But many records were filled out in error, he contends. In a review of 1,500 procedures performed by one neurosurgeon, this individual was listed as an attending 50 percent of the time and as either a surgeon or assistant the other 50 percent of the time. In 746 other cases, the error rate was 100 percent. When queried, Winn says, all nurses stated that in such complex cases the attending (that is, the faculty member) was always present. Clearly, the record keeping by the nurses varied greatly and was unreliable as an indicator of an OR presence. That error was compounded as the information moved through the billing process, and not only were the correct names of some doctors left off records, the names of doctors who werent in attendance were added. Again, Winn suggests this was all done unintentionally. However, Recognition that the government may hold individual faculty members responsible for errors rather than universities and practice plans is a strong inducement to get it right the first time, the convicted felon adds.