Most people don’t think about the government when they step on the scale. But the government, apparently, is thinking of you.
Last month, state and federal officials delivered a torrent of ominous warnings about the “epidemic” of obesity. On the very same day that the press carried reports of Southwest Airlines requiring “people of size” to purchase an extra seat, the state Department of Health announced that the number of local obese people has doubled in just 10 years, to 18.5 percent of the population. Add to that the number who are simply overweight (but not obese), according to the Health Department figures, and you get more than half of the population that could be considered fat.
Nationally, an incredible 61 percent of the population is in that category, the feds recently scolded, as President Bush launched a new crusade on fat. And not only did the government remind us that the overweight are at greater risk of developing heart disease, diabetes, and other diseases, but it declared obesity in itself a disease, the treatment of which now qualifies as a tax deduction.
“We’ve never seen an epidemic of chronic disease go across the country like this so quickly,” says Ali Mokdad, an epidemiologist for the Centers for Disease Control, using the prevailing terminology, which he points out the CDC doesn’t use lightly.
There’s a certain gleefulness with which many of us greet news of our compatriots’ flabbiness. It’s an opportunity to feel superior to those, we imagine, with poor self-restraint and worse taste, eating their way to an early grave on Big Macs and Chee*tos. Yet the alarmism invites skepticism. Fat is a disease? An epidemic? Is it really that bad? Well, yes and no. Significantly, one thing most government and press reports neglect to mention is that the official definition of fat has changed in recent years.
In 1998, the National Institutes of Health came up with new guidelines based on a complicated height-weight calculation that determines something called the “body mass index” or BMI. (Your BMI is your weight in kilograms divided by height in meters squared; to get yours quickly, go to the BMI calculator at www.nhlbisupport.com/bmi.) Before, the government didn’t call you overweight until, if you were a woman, you had a BMI of 27.3 (164 pounds for someone 5-foot-5) or if a man, 27.8 (205 pounds for a 6-footer).
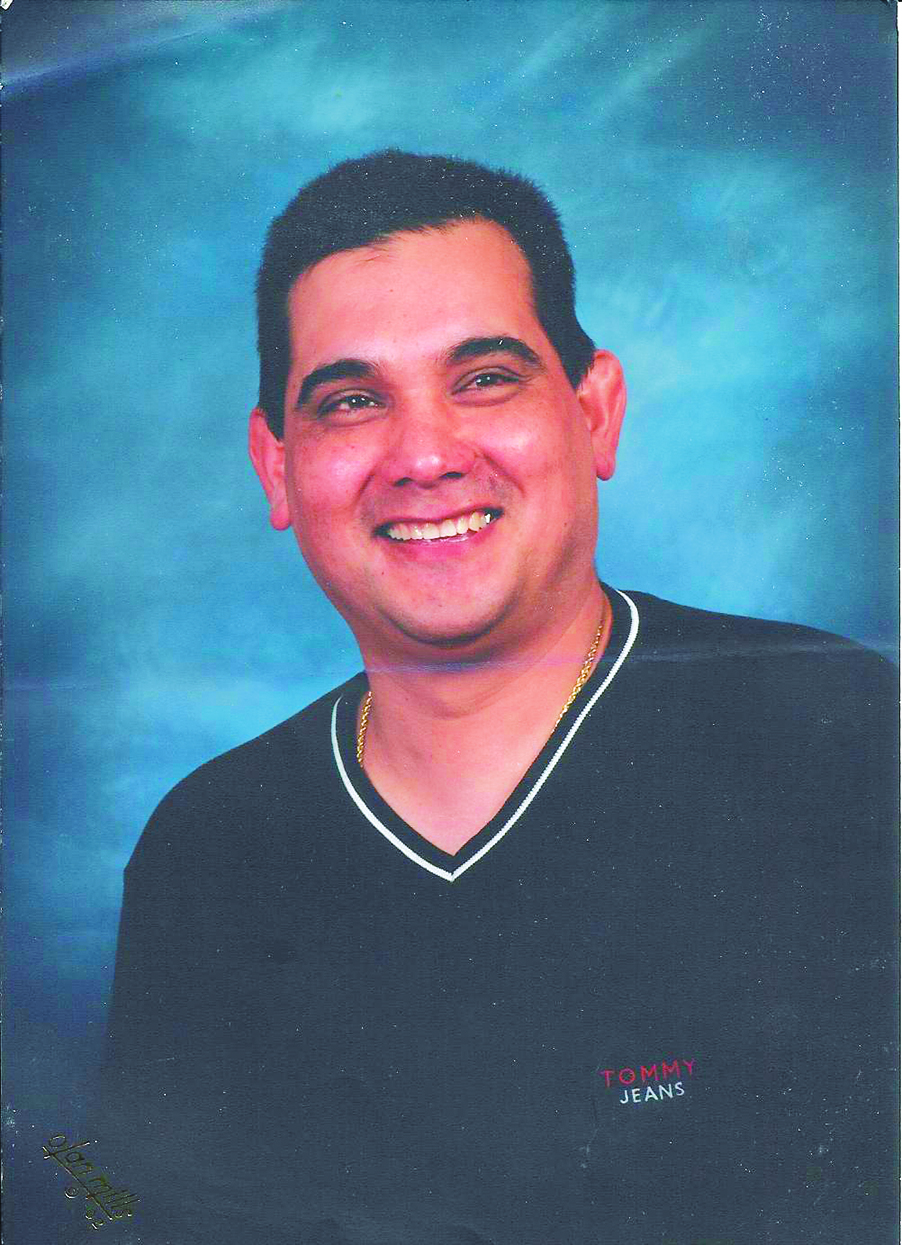
Now you’re officially overweight once you hit a BMI of 25, whatever your ![]()
![]() gender (for someone 5-foot-5, that’s 150 pounds; for someone 6-foot, 184 pounds). Obesity, previously not precisely quantified, now sets in at a BMI of 30 (180 pounds for the 5-foot-5 person, 221 pounds for the 6-foot- tall individual).
gender (for someone 5-foot-5, that’s 150 pounds; for someone 6-foot, 184 pounds). Obesity, previously not precisely quantified, now sets in at a BMI of 30 (180 pounds for the 5-foot-5 person, 221 pounds for the 6-foot- tall individual).
Local and national health officials are quick to point out that, in looking at weight gain over the past decade, they are comparing apples to apples. Having databases of height and weight figures from past years at their disposal, they retroactively apply the new guidelines to come up with figures they can compare to current numbers.
“No matter how you look at the data, it would still be worse,” says David Solet, a King County epidemiologist who helped prepare a separate county report that was released this spring. The county’s population put on an average of 11 pounds between 1987 and 2001. Even in a part of the country populated by hikers and bikers, flab is everywhere.
While their figures support the claim that Americans have gotten fatter, it isn’t clear that most of us can actually be called fat, nor that a majority of the populace has significant health risks because of their weight. Just how big a problem we are perceived to have, in fact, is dramatically inflated by the new guidelines.
State epidemiologist Juliet Eenwyk insists that, whether you use the old or new guidelines, about half of the state’s population would be considered overweight. But that’s inconsistent with most findings.
In 1998, King County determined that the new guidelines doubled the number of county people judged to be overweight or obese, from 24 percent to 48 percent. Nationally, when the new guidelines came out, the percentage of the population who were officially fat jumped from 35 percent to 55 percent.
The guidelines change arouses suspicion. David Levitsky, a Cornell University professor of nutrition and psychology who believes that obesity is a serious problem, nonetheless notes, “A lot of people make a lot of money on big people.” The pharmaceutical and weight-loss industries have a financial interest in pushing the fat criteria downward, Levitsky says, and the reach of those industries can be felt even among the type of scientific “experts” who came up with the new guidelines. Such scientists frequently act as consultants for drug companies that make diet pills. Much academic research is funded by drug companies as well. How much better a case it makes for their weight-loss products if flab is presented as a health, not just aesthetic, problem. And how much easier for scientists to get grant money to study the issue.
Yet, the guidelines are supported by a body of research that points to the ill effects of weight even among people not previously thought of as heavy. One often cited study, by Harvard nutritionist JoAnn Manson and others, found an increased death rate due to coronary disease among middle-aged women with a BMI as low as 22, which translates into a slim 132 pounds for a 5-foot-5 woman. She further noted that among women who never smoked, the lowest overall mortality was had by those with a BMI of under 19, which renders a woman of the same height with the modellike weight of 114 pounds.
Journalist Michael Fumento, author of the book Fat of the Land, says the evidence from studies like Manson’s is clear, no matter how depressing: “Short of starvation, the thinner you are, the healthier.” The message filters down through local pronouncements like this one, in King County’s spring report: “Even a moderate weight gain of 10 to 20 pounds for a person of average height can increase the risk of death.”
If that seems like a loaded message to unleash on a country that, for all its flabbiness, is obsessed with weight (remember anorexia, anyone?), it’s also one that may overstate its case. In the Manson study, the death rate for what would now be termed the “mildly to moderately overweight women” (with BMIs between 25 and 29) was, while higher than those of thinner women, still extremely low. Only 4.5 percent of those women died of anything at all, never mind a disease linked to weight.
“The medicalization of food and weight has gotten completely out of control,” concludes Cornell French professor Richard Klein, author of the argumentative book Eat Fat. It has, he says, “led people to believe that if they put on a few pounds, they are doing something bad for their health,” when “in practical terms, the additional risk is infinitesimal, particularly in light of the other dangers we face.”
The health risks do increase starkly among the truly obese. King County’s spring report shows that 29 percent of obese county residents over 65 have diabetes, four times as many as the “healthy weight” seniors. An overwhelming 67 percent of obese seniors have high blood pressure, while only 37 percent of their thin counterparts do.
Even when considering the obese, though, some question whether such health risks are due to weight per se, or to associated factors like diet and exercise. They look to recent work by the Cooper Institute of Dallas, which put research subjects on a treadmill to test their fitness. Those who were fit, even if they were obese, had a lower mortality than those who weren’t, no matter if thin.
That’s important, says “fat but fit” guru Glen Gaesser, a professor of exercise physiology at the University of Virginia, because many people aren’t going to be able to reach their ideal weight. Genetics and pesky fat cells, accumulated over years of unhealthy living, conspire against those trying to lose weight, who shed on average only four to seven pounds. His solution: Exercise, eat well, and “let the pounds fall where they may.” It may not make either the government or the diet industry happy, but he and others believe you can still be healthy.
It’s also, of course, a more relaxed way to live. Eat Fat author Richard Klein, who is living in Paris at the moment, observes that whereas Americans constantly worry about what they eat, the French eat for pleasure. Happily influenced by the French, he now finds himself eating both better and less.